Key Takeaways
-
Medicare Advantage plans with poor star ratings often hide their most restrictive policies in the fine print, including narrow provider networks, prior authorization rules, and unexpected cost-sharing.
-
In 2025, choosing a plan based only on advertised benefits can lead to serious limitations in care when you need specialists, procedures, or out-of-network options.
Why Fine Print Is Where the Worst Surprises Lurk
When you review a Medicare Advantage plan, the glossy brochures and TV ads may highlight perks like dental, vision, and gym memberships. But those extras are often distractions. What really matters is in the fine print: the coverage restrictions, costs, and rules that could directly affect your care.
The worst Medicare Advantage plans in 2025 still get away with deceptive impressions because too many enrollees overlook these crucial details. If you’re like many beneficiaries, you may focus on the monthly premium and overlook:
-
Prior authorization requirements for tests and treatments
-
Limitations on provider networks
-
Caps on out-of-network coverage
-
Vague or delayed appeal processes for denied claims
Reading every section of the Summary of Benefits, Evidence of Coverage, and Plan Annual Notice of Change is essential before enrollment.
What Star Ratings Reveal (and What They Don’t)
CMS rates Medicare Advantage plans on a 5-star scale based on metrics like customer service, care quality, and member experience. While it’s helpful to avoid plans rated below 3 stars, even plans with 3.5 or 4 stars may contain hidden drawbacks.
Plans rated 2.5 stars or below are subject to potential contract termination by CMS. If you see one of these plans still available in your area, treat it as a red flag. Even a 3-star rating in 2025 should prompt a deeper look into:
-
Complaint volume from members
-
Delays in getting care approved
-
Changes to coverage year over year
Star ratings are only a starting point, not a guarantee of quality or access.
Narrow Networks Are a Common Tactic
Some of the worst-performing Medicare Advantage plans operate with extremely limited provider networks. In practice, this means your preferred doctor, hospital, or specialist may not be covered.
In 2025, some plans limit you to only a few in-network facilities, especially in rural or suburban areas. This becomes a serious issue if:
-
You develop a complex condition and need a specialist
-
Your primary care provider leaves the network mid-year
-
Your closest hospital isn’t contracted with your plan
Always check the provider directory, and don’t assume a provider listed in 2024 is still participating in 2025.
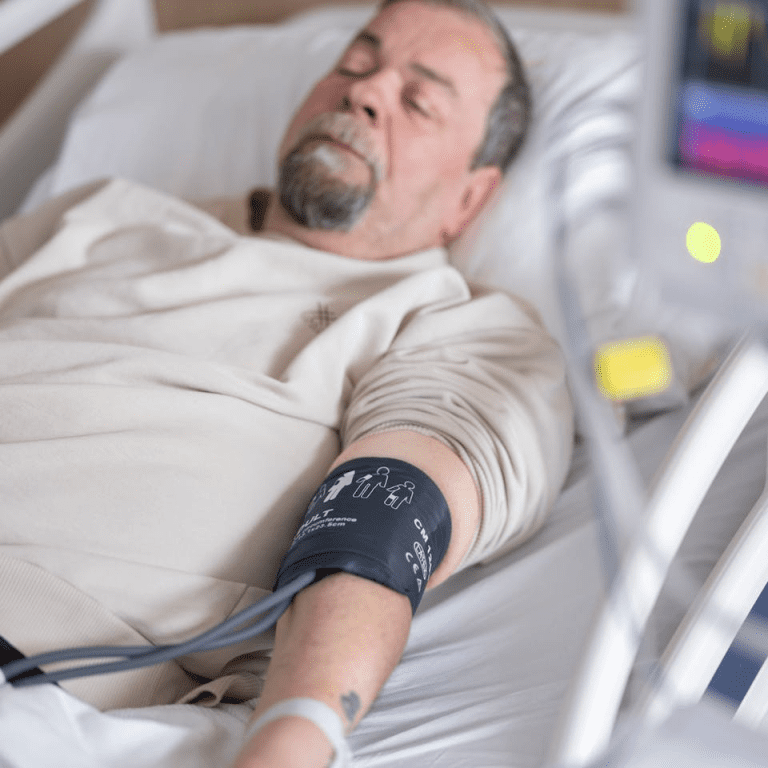
Prior Authorization Is a Silent Barrier
Many Medicare Advantage plans require prior authorization before approving certain services, such as MRIs, outpatient surgery, or home health care. While this is not unusual, the worst plans use it excessively, leading to delays or denials in medically necessary care.
In fact, recent reviews by CMS and the Office of Inspector General have confirmed that some plans improperly deny care that should be covered. In 2025, look for these warning signs:
-
Over 50% of high-cost services require prior approval
-
Complex approval processes with long wait times
-
Appeals processes that take more than 30 days
Prior authorization should not become a gatekeeping tool for denying benefits you’re entitled to.
Appeals Are Slow and Confusing
If your plan denies a treatment or service, you have the right to appeal. But the worst Medicare Advantage plans make this process unnecessarily difficult.
You may experience:
-
Confusing paperwork
-
Lack of guidance from customer service
-
Extended timelines beyond the 14–30 day window CMS allows for reconsideration
In 2025, you can expect better oversight from CMS, but low-performing plans often test the limits of these regulations. If your health deteriorates during a delay, you may not get the care you need in time.
Out-of-Pocket Limits Are Often Misleading
Medicare Advantage plans must include a maximum out-of-pocket (MOOP) limit for in-network services. In 2025, the in-network MOOP limit is capped at $9,350, with combined in- and out-of-network limits reaching up to $14,000. But here’s where the fine print matters:
-
Only in-network services apply to the lower limit
-
Out-of-network care may be limited or not covered at all
-
Prescription drug costs have a separate $2,000 cap under Part D, but this doesn’t count toward medical MOOP
Some plans market low in-network MOOPs but have high rates of out-of-network denial, making those limits nearly irrelevant for many beneficiaries.
Extra Benefits Distract from Core Weaknesses
Plans often promote non-medical perks like transportation, meal delivery, or over-the-counter items. These are helpful, but they don’t substitute for robust medical coverage.
In 2025, plans that focus too heavily on perks often:
-
Cut corners on network quality
-
Enforce stricter prior authorization rules
-
Use aggressive cost-control tactics that limit access to needed care
Evaluate extra benefits only after confirming your plan has strong medical and hospital coverage.
Annual Changes Create Confusion
The terms of Medicare Advantage plans can change every year. What looked like a decent option in 2024 may now have:
-
A reduced provider network
-
A higher deductible or copay schedule
-
New prior authorization requirements
By October, you should receive the Annual Notice of Change (ANOC). The worst plans often bury major reductions in this document. You have until December 7 to make a change during Medicare Open Enrollment, so don’t overlook this critical review window.
Red Flags to Watch For in 2025
When reviewing plans this year, pay attention to these warning signs:
-
A history of star ratings under 3.5
-
Minimal transparency about prior authorizations
-
Limited or unclear information about appeals
-
High out-of-pocket limits with vague network rules
-
Overemphasis on perks instead of core benefits
Use Medicare Plan Finder or speak with a licensed agent listed on this website to get a second opinion before you enroll.
What You Should Do Before Enrolling
Protect yourself by reviewing:
-
Star Rating: Look for 4 stars or higher, but don’t stop there.
-
Provider Directory: Confirm your doctors and hospitals are in-network.
-
Drug Formulary: Make sure your prescriptions are included.
-
MOOP Limit: Understand both in-network and out-of-network limits.
-
Prior Authorization Rules: Ask how many services require approval.
-
Evidence of Coverage: Read this document fully before signing up.
Make sure all this information reflects 2025 updates. Even small changes can affect your total costs and access to care.
Why Scrutiny Matters More in 2025
Medicare Advantage enrollment has grown rapidly over the past few years, and 2025 continues this trend. But as enrollment grows, so does scrutiny. Regulators are paying closer attention to plan performance, denials, and marketing.
Still, poor-quality plans often survive because many enrollees don’t fully understand what they’ve signed up for until it’s too late. By staying proactive and informed, you can avoid this mistake.
Your Plan Should Work for You, Not Against You
Choosing a Medicare Advantage plan in 2025 means balancing cost, care quality, and flexibility. The worst plans tilt that balance away from you, often hidden in the fine print.
Don’t let marketing gloss over critical flaws. Take the time to read the full documentation, verify your provider access, and understand your rights when something goes wrong.
If you’re uncertain about your options or confused by the plan language, speak with a licensed agent listed on this website. Their insights can help you avoid costly surprises.