Key Takeaways
-
In 2025, Medicare covers more mental health services than ever before, including therapy from marriage and family therapists and mental health counselors. But eligibility, timing, and provider rules still apply.
-
Delaying care can create unnecessary barriers. Understanding enrollment windows, annual limits, and in-person requirements helps you avoid gaps in mental health coverage.
A Stronger Focus on Mental Health in 2025
Medicare’s approach to mental health has significantly improved in 2025. After years of advocacy and policy changes, you now have broader access to critical services like therapy, psychiatric evaluations, and medication management. Most importantly, Medicare now recognizes mental health as a vital part of your overall healthcare.
But while the system is more inclusive, the timing of when you seek care still affects your access. Waiting too long to act, misunderstanding eligibility, or missing enrollment periods can delay treatment and increase out-of-pocket costs.
What Medicare Covers for Mental Health in 2025
Medicare offers different types of mental health support depending on the setting and the kind of provider. Here’s what you’re entitled to in 2025:
Inpatient Care (Medicare Part A)
If you’re admitted to a hospital for a mental health condition, Medicare Part A covers:
-
Up to 190 days of inpatient psychiatric care in a standalone psychiatric hospital over your lifetime.
-
Unlimited days in a general hospital.
-
Room and meals, nursing care, medications, and therapy while admitted.
Outpatient Services (Medicare Part B)
Medicare Part B covers services like:
-
Individual and group therapy
-
Psychiatric evaluations and medication management
-
Partial Hospitalization Programs (PHP)
-
Intensive Outpatient Programs (IOP)
-
Screenings for depression and substance use
You pay 20% of the Medicare-approved amount after you meet the annual Part B deductible ($257 in 2025).
Mental Health Providers You Can See
You are no longer limited to only psychiatrists or clinical psychologists. As of 2025, you can also receive therapy from:
-
Licensed clinical social workers (LCSWs)
-
Clinical nurse specialists
-
Nurse practitioners
-
Physician assistants
-
Marriage and family therapists (MFTs)
-
Mental health counselors (MHCs)
These additions mean shorter wait times and more provider options, but you must confirm they accept Medicare.
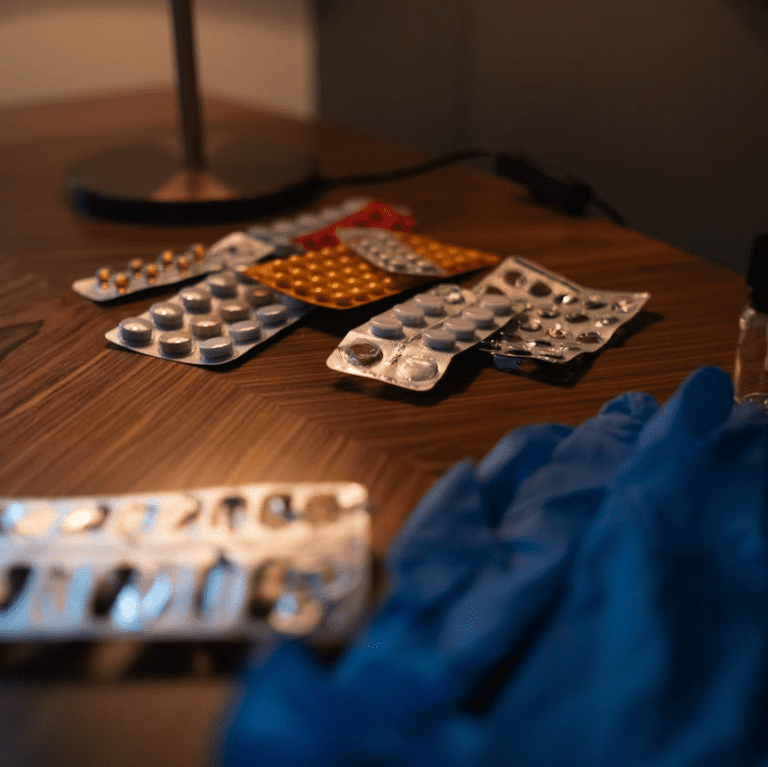
Prescription Drugs (Medicare Part D)
Part D plans cover medications used to treat mental health conditions, such as antidepressants, antipsychotics, and anti-anxiety medications. In 2025, there is a $2,000 cap on out-of-pocket spending for covered prescription drugs, which brings significant relief if you need ongoing medication.
Don’t Miss These Critical Timelines
While Medicare covers a lot, timing matters more than ever. Missing certain windows could leave you without access or lead to costly delays in care.
Initial Enrollment Period (IEP)
When you first become eligible for Medicare (usually around age 65), you have a 7-month window:
-
Begins 3 months before the month of your 65th birthday
-
Includes the month you turn 65
-
Ends 3 months after that month
Enroll during this period to avoid late penalties and gaps in mental health coverage.
General Enrollment Period (GEP)
If you missed your IEP, the GEP runs from January 1 to March 31 each year. Coverage starts July 1. You might face late enrollment penalties, and your access to therapy and psychiatric care will be delayed until coverage begins.
Annual Enrollment Period (October 15 to December 7)
Each year, you can make changes to your Medicare Advantage or Part D plan. If you’re using therapy or psychiatric drugs, this is the time to:
-
Review your plan’s mental health provider network
-
Ensure your medications are still covered
-
Avoid coverage lapses that can interrupt treatment
Special Enrollment Periods (SEP)
You may qualify for a SEP if you experience life events such as:
-
Losing employer coverage
-
Moving to a new area
-
Being diagnosed with a chronic mental illness
A SEP lets you make mid-year changes without waiting until October.
In-Person Visit Rule for Telehealth
Medicare permanently covers telehealth visits for mental health. However, starting October 1, 2025, you must have an in-person appointment with your provider every 12 months to continue receiving mental health services via telehealth.
-
Exceptions apply if travel is a hardship or you live in a rural area
-
If you skip this in-person visit, telehealth coverage could be paused
How Medicare Advantage Plans Fit In
All Medicare Advantage (Part C) plans must cover at least the same mental health benefits as Original Medicare. Some plans offer extra features, such as:
-
Expanded therapy sessions or longer appointment times
-
Care coordination between your therapist, primary doctor, and specialist
-
Extra wellness or behavioral coaching programs
But each plan has its own network, rules, and costs. If you’re already in therapy, switching plans could affect your provider access. Always confirm with your plan before making changes.
Choosing the Right Mental Health Provider
Finding a provider who fits your needs and accepts Medicare can still take time. To avoid delays:
-
Use Medicare’s online provider search tool
-
Contact your plan for a directory of in-network therapists
-
Call ahead to confirm the provider is still accepting Medicare patients
MFTs and MHCs are new additions in 2025, so not every office may be familiar with billing Medicare. Be patient but persistent.
What Happens if You Wait Too Long
Even though coverage is available, here’s what can happen if you wait too long to get care:
-
Missed enrollment: If you delay signing up for Medicare or a Part D plan, you could go months without coverage for therapy or psychiatric medications.
-
Provider shortages: Many Medicare-accepting therapists book out months in advance. Waiting can limit your choice of therapists or delay your first appointment.
-
Telehealth interruptions: If you forget to schedule your required in-person visit before October 2025, you might lose access to remote therapy sessions.
-
Emotional toll: Delaying care can make your condition worse, increasing the time and intensity of treatment needed later.
Mental health care works best when started early and consistently maintained. Don’t wait until things get worse before reaching out.
Medicare and Preventive Mental Health
In addition to treatment, Medicare Part B also covers preventive services:
-
Annual depression screening with a primary care provider
-
Alcohol misuse screening and counseling
-
Tobacco use cessation counseling
These services cost you nothing if provided by a Medicare-assigned provider. Taking advantage of them can help you address issues before they become more serious.
Making Medicare Work for Your Mental Health in 2025
To make the most of your Medicare mental health benefits this year:
-
Enroll on time: Don’t miss your IEP or annual plan review period
-
Know your deductible: In 2025, Part B’s deductible is $257, after which you pay 20%
-
Choose wisely: If considering a Medicare Advantage plan, check the provider network for therapists and mental health clinics
-
Track your coverage: Know how many sessions are covered and whether pre-authorization is needed
-
Stay in touch with providers: Schedule your annual in-person visit to maintain telehealth access
Even with expanded benefits, Medicare won’t automatically connect you to care. You have to take the first step, stay aware of timelines, and choose plans and providers that match your needs.
Take Action to Protect Your Mental Health Access
Medicare in 2025 gives you the tools, but it’s up to you to use them. Every month or year you delay treatment could result in more complex, costlier care later. Understanding your enrollment period, provider options, and benefit rules helps you get care when you need it most.
Don’t wait until your condition becomes harder to manage. Talk to a licensed agent listed on this website for help reviewing your options, understanding timelines, and finding the right plan for your mental health care.