Key Takeaways
-
Missing your Initial Enrollment Period (IEP) or misunderstanding its rules can lead to lifelong late enrollment penalties and limited coverage options.
-
In 2025, the IEP remains the most critical window for avoiding extra costs, especially with changes in Medicare Part D and increased reliance on integrated coverage.
Your Initial Enrollment Period: What It Is and Why It Matters
If you are approaching age 65 in 2025, the most important Medicare deadline you’ll face is your Initial Enrollment Period (IEP). This is your first opportunity to enroll in Medicare, and it only happens once. Missing this window can result in lifelong penalties and delays in coverage.
Your IEP begins three months before the month you turn 65, includes your birth month, and extends for three months after. That makes for a seven-month window total. But not all seven months offer the same outcome. If you delay until the last few months of your IEP, your coverage might not start until months later—leaving you exposed.
In 2025, with Medicare’s updated drug coverage rules and out-of-pocket protections, enrolling at the right time is more important than ever.
What Happens If You Miss Your IEP?
Failing to sign up for Medicare Part B or Part D when you’re first eligible can lead to the following issues:
-
Late Enrollment Penalties
-
For Part B: 10% added to your premium for every 12-month period you delayed.
-
For Part D: 1% added for each month you went without creditable drug coverage.
-
-
Gaps in Coverage
-
Missing your IEP means you may have to wait for the General Enrollment Period (January 1 to March 31) the following year, with coverage not beginning until July 1.
-
-
Limited Plan Options
-
Outside your IEP, you may face restrictions in plan choice or underwriting for Medigap plans.
-
These penalties are often permanent and cumulative, which means you could overpay for Medicare for the rest of your life.
Who Needs to Enroll During Their IEP?
You should enroll during your IEP unless you have active creditable coverage through current employment (yours or your spouse’s). Retiree coverage, COBRA, or TRICARE for Life typically do not qualify as active employer coverage for delaying Part B or Part D enrollment without penalty.
If you’re still working at age 65 and covered by a group health plan:
-
You can often delay Part B and Part D without penalty.
-
Once your employment or group coverage ends, you’ll receive a Special Enrollment Period (SEP), typically lasting 8 months for Part B and 63 days for Part D.
Without employer coverage, you must enroll during your IEP to avoid penalties and gaps.
IEP Timing and Coverage Start Dates
Understanding how your enrollment timing affects coverage start dates is crucial. In 2025, coverage start rules are as follows:
-
If you enroll during the 3 months before your birth month, coverage starts on the first day of your birth month.
-
If you enroll during your birth month, coverage starts the first day of the next month.
-
If you enroll in the 3 months after your birth month, coverage starts the first day of the following month.
This is a change from pre-2023 rules when late IEP enrollments could delay coverage by up to three months.
The Part D Mistake That Still Catches People in 2025
In 2025, Part D includes a new $2,000 annual out-of-pocket cap and a payment smoothing option. But if you delay enrolling in Part D and lack other creditable drug coverage, you still face the same penalties as before.
People often skip Part D because they aren’t taking prescriptions at age 65. That logic backfires quickly:
-
Any month without creditable coverage adds to your Part D penalty.
-
Even if you join a plan later, you’ll pay the penalty monthly—for life.
-
You could be locked out until the next Annual Enrollment Period (October 15 – December 7).
How Medigap and Advantage Plans Tie Into Your IEP
Medicare Supplement Insurance (Medigap) and Medicare Advantage (Part C) plans also depend on your IEP for guaranteed access.
-
Medigap: You have a one-time 6-month Medigap Open Enrollment Period starting the month you’re both 65 and enrolled in Part B. During this period, insurance companies can’t deny you coverage or charge more due to preexisting conditions.
-
Medicare Advantage: Your IEP also allows you to enroll in a Medicare Advantage plan. If you miss it, you typically have to wait until Annual Enrollment Period unless you qualify for a Special Enrollment Period.
Delays or mistakes here can cost you in both premiums and benefits.
What Counts as Creditable Coverage for Part D?
To avoid the Part D late penalty, you need drug coverage that’s considered creditable—meaning it’s expected to pay on average as much as Medicare’s standard drug coverage.
Examples of creditable coverage include:
-
Employer or union plans with prescription benefits
-
VA drug coverage
-
Some retiree coverage
-
Some individual private plans (verify status in writing)
If your plan isn’t creditable or you aren’t sure, request a Notice of Creditable Coverage from your provider.
You Can’t Assume You’ll Be Notified
In 2025, Medicare continues to send welcome packages and reminders—but they won’t track your employer coverage or personally notify you if you miss your window. You’re responsible for knowing your IEP and taking action.
Common assumptions that lead to mistakes:
-
Believing Social Security will enroll you automatically
-
Thinking COBRA or retiree plans count as active coverage
-
Assuming you can enroll anytime without penalties
Unless you’re already receiving Social Security or Railroad Retirement Board benefits, you must actively sign up for Medicare.
Avoiding Enrollment Mistakes in 2025
Here are a few smart actions you can take to avoid costly IEP mistakes:
-
Mark your calendar at least 6 months before your 65th birthday.
-
Talk to your employer’s HR department about your plan’s Medicare coordination.
-
Check whether your drug coverage is creditable in writing.
-
Enroll early in your IEP if you know you’ll need Medicare.
-
Review your plan choices with a licensed agent listed on this website to avoid overpaying.
In 2025, proactive planning is essential. With changes to Part D and more coordination between Medicare and other coverage types, missteps are easier to make and harder to correct.
The General Enrollment Period Isn’t a Safety Net
If you miss your IEP entirely and don’t qualify for a Special Enrollment Period, your next chance is the General Enrollment Period (GEP) from January 1 to March 31.
-
You can enroll in Part A and/or Part B during this time.
-
Coverage begins the first day of the month after you enroll.
-
Late penalties still apply.
This means you could go without Medicare coverage for several months and still pay more once enrolled.
Why Overpayment Often Lasts for Life
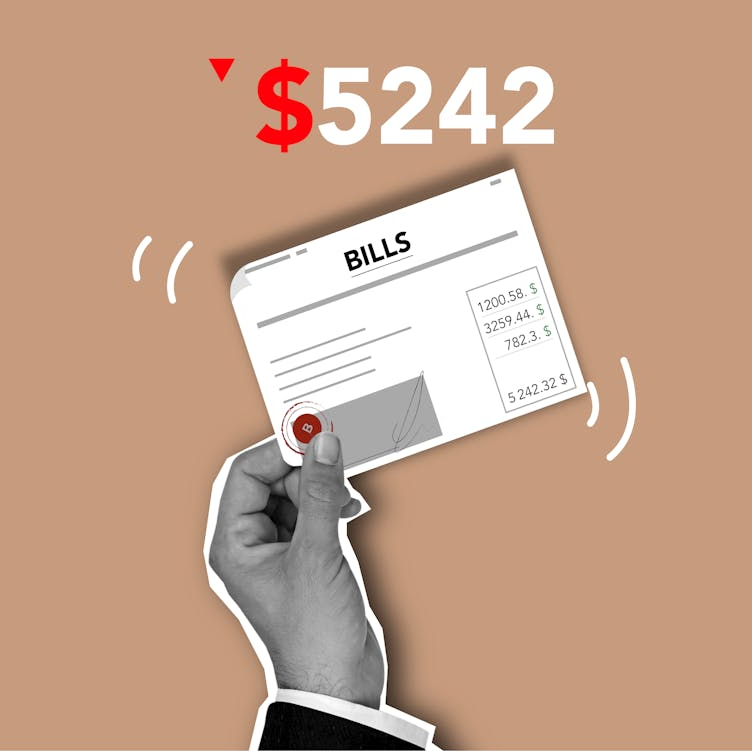
Late penalties are calculated monthly but charged every month for the rest of your life. Over time, even a small monthly surcharge adds up to thousands of dollars. This is particularly true with:
-
Part B Penalty: 10% per 12-month delay. If you delay 3 years, that’s 30% more—permanently.
-
Part D Penalty: 1% per month of delay, calculated off the national base premium (which may change annually).
And those are just the penalties. Missing your IEP may also cost you access to:
-
Lower premiums
-
Broader provider networks
-
Guaranteed issue rights for Medigap
Stay Ahead of the Clock, Not Behind It
Your Initial Enrollment Period in 2025 is your one-time opportunity to get Medicare right from the start. Mistakes during this window can be expensive, permanent, and limiting.
-
Know your 7-month IEP timeline.
-
Act early to prevent coverage gaps.
-
Understand how Part B and D penalties work.
-
Confirm if your other insurance qualifies as creditable.
If you’re unsure or overwhelmed, there’s help available.
Don’t Pay More Than You Need To
The most avoidable Medicare mistakes often come down to one thing: timing. The right time to act is before your IEP ends—not after penalties begin. Getting advice from someone who understands the rules can prevent you from paying more than you should.
Speak with a licensed agent listed on this website to review your enrollment options, confirm your timeline, and ensure you aren’t leaving benefits or dollars on the table.